Photo Credit: everything possible / Shutterstock.com
Causes of Fibromyalgia
Even as more advancements are made in fibromyalgia treatment, the disease is still one of the most mysterious known to the medical community. Symptoms can come suddenly or gradually, and could congregate in one physical area or spread throughout your body. As if the nagging symptoms weren’t frustrating enough, the lack of a distinct, measurable source makes treatment a game of trial and error.
There are conflicting theories about where fibromyalgia comes from, but doctors do agree that the condition probably rests on a combination of causes, and those causes are often interrelated. Here are some medically-supported ideas on what causes fibromyalgia, and although they have not been scientifically proven, you might want to consider if any may be playing a role in your case.
1. Genetics
There is no definitive proof that fibromyalgia is genetic, but there certainly seems to be a hereditary pattern. One study from 2008 followed pairs of twins over several years, and determined that the risk of developing chronic pain was at least 50% genetic; another study conducted in 2004 found that people were eight times as likely to develop fibromyalgia if they had a relative who suffered from it. Although a specific “fibromyalgia gene” has not been found yet, experts have linked several gene variants to the condition, which supports the genetic component theory.

Photo Credit: Volt Collection / Shutterstock.com
2. Traumatic Events
Physical trauma – especially injuries to the head, neck or spine – has been known to trigger fibromyalgia symptoms. Research shows that adults with neck trauma are more than 10 times as likely to develop fibromyalgia within one year as people who experienced fractures or injuries in their lower extremities. Invasive surgery is another possible trigger, but it’s unclear whether the physical trauma of the procedure is to blame, or if the sleep problems and low activity levels during recovery exacerbate fibro symptoms. Some infections can have lasting neuromuscular effects that may also lead to fibromyalgia, such as Lyme disease, streptococcus virus, and HIV.
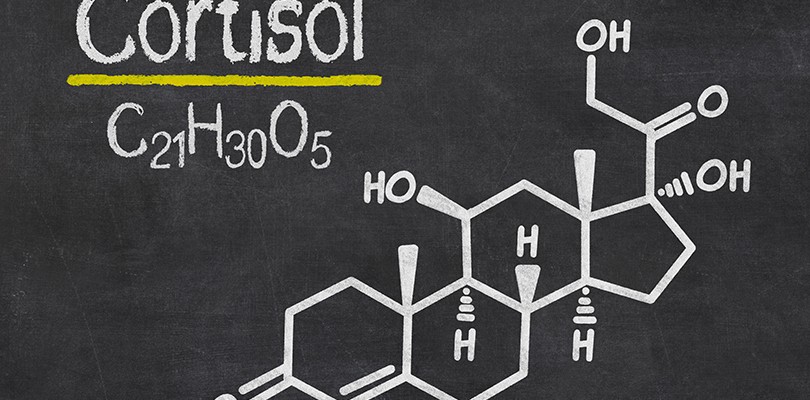
Photo Credit: Zerbor / Shutterstock.com
3. Hormonal Imbalance
Many fibro patients have low levels of important hormones like cortisol and androgens, and some experts believe this imbalance is the major source of the disease. The theory centers on the fact that certain hormones support muscle growth, helping the body metabolize important vitamins and minerals for better muscle and brain function. And while there isn’t concrete evidence that hormonal issues are to blame, hormone blood tests have been used as diagnostic markers in certain cases, and some fibro patients have found significant relief with bio-identical hormone replacement therapy (BHRT).

Photo Credit: Umpaporn / Shutterstock.com
4. Vitamin Deficiencies
Healthy muscle function rests on the right balance of minerals and vitamins in your cells – something that can be difficult to track by yourself. Although it may not clear up all of your symptoms, topping up your levels of magnesium, vitamin B12 and vitamin D often can have a profound effect on pain and fatigue, which suggests that a severe vitamin deficiency could be at the root of fibromyalgia. Leaky gut syndrome is a related cause, where problems with the mucus membranes of your intestines make vitamin absorption difficult, food intolerances more likely, and widespread viral infection possible.
There are signs, symptoms and statistics outside of the hallmarks of fibromyalgia that are not as frequently reported but just as important to recognize.
Photo Credit: Creations / Shutterstock.com
5. Brain Chemistry
Fibro patients tend to have lower levels of certain neurotransmitters and endorphins, which may leave them more vulnerable to pain. Serotonin, a neurotransmitter responsible for calming the mind and muscles, is lacking in the fibro brain, as is growth hormone (critical for maintain and repairing muscle), and the endorphins that act as natural painkillers. On top of these deficiencies, doctors have found an increase in the chemical known as “substance P”, which amplifies pain signals.

Photo Credit: Dirima / Shutterstock.com
6. Muscle Microtrauma
In contrast to an abrupt muscle tear or strain, “microtrauma” refers to very slight muscle damage that can come from hypoxia, prolonged muscle spasm, local muscle abnormalities, or ischemia (restricted blood supply to the tissues). This can develop from an injury, but is more likely to come from a muscle imbalance: problems with circulation cause a drop in pH and muscle enzymes to stop functioning properly, which depletes energy and can lead to these tiny structural changes that interrupt normal function. Some studies have found evidence of microtrauma in muscle biopsies of fibro patients, which could help to explain the deep muscle pain.
Photo Credit: Stokkete / Shutterstock.com
7. Chronic Stress
Stress has been flagged as a source of inflammation, hormone imbalance, poor recovery, and a host of other ailments. In fact, chronic stress is so disruptive to your body and sleep cycle that some experts believe it to be the main culprit behind several serious diseases, including chronic pain conditions. A few aspects of the stress response may be at play, including an overactive adrenal gland (resulting in adrenal fatigue), poor regenerative rest (known as stage 4 sleep), and emotional tension. Ultimately, prolonged stress can lead to a domino effect, eventually interfering with all your body’s natural processes – including pain response.
Learn more about how fibromyalgia works over at NewLifeOutlook.
When people talk about fibromyalgia pain, they may use the terms tender points and trigger points, but what is the difference between the two?